
Sometimes referred to as autologous conditioned plasma (ACP) therapy, platelet-rich plasma (PRP) therapy has increasingly been used for various orthopedic conditions, including chronic arthritis. With no definitive curative therapy, the use of PRP in the treatment of osteoarthritis has been a topic of research and advancement.
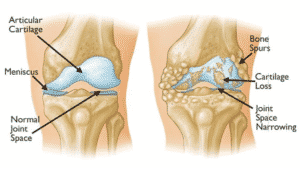
Osteoarthritis is the condition when the cartilage is diminished. Cartilage provides a cushion so the joints don’t come in contact. But without a cushion, the joint bones can rub each other. Especially when there is movement or shock to a joint, cushion is needed to avoid pain and the formation of bone spurs. When osteoarthritis is present, we often see swelling, stiffness, and pain in the patient.
What is PRP?
PRP is an autologous blood product that has a high concentration of platelets (2.5-9 times greater than whole blood) obtained by centrifuging a sample of the patient’s blood.
Platelets do not have any restorative or healing properties, but rather secrete growth factors and proteins which play a critical role in maintaining tissue homeostasis and regulating the inflammation and coagulation response of the body.
PRP therapy has been found to modulate chondrocyte apoptosis inhibition, bone and vessel remodeling, inflammation modulation, and collagen synthesis.
Who are the candidates?
Since PRP is a new therapy, with a large volume of ongoing studies and data to analyze, there is a consensus forming regarding appropriate criteria or indications for PRP use.
Studies suggest the use of PRP therapy for arthritis to be more beneficial in patients with early degenerative arthritis, who have unsuccessfully tried other management options like NSAIDs and physical therapy and are not ready for joint replacement surgeries.
Healthy patients are the best candidates, as a biologic product from the patient’s blood. The healthier you are, the better chance these treatments are likely to succeed.
Oftentimes, the patient wishes to try all safe options prior to the decision to have surgery.
Due to the newness of PRP therapy, it is not covered by Medicare or commercial insurance plans, such as Blue Cross Blue Shield. So candidates for PRP currently must have the means for paying for the treatment, although some health care financing plans may be an option.
Who should avoid PRP injections?
Patients with medical illnesses which can worsen with injection like active infections, bleeding disorders, patients on anticoagulant therapy, anemia, and pregnant women should avoid PRP injections.
PRP for Knee Osteoarthritis
Arthritis in the knee can be debilitating. It is often caused by too much weight on the knee, an injury to the knee, or even an infection that can reduce cartilage. But osteoarthritis can merely be the result of age or heredity.
Knee arthritis is more common in women, and while it can occur at a young age, most patients are over 45 years old. Options for treating knee osteoarthritis include:
- PRP Therapy
- Losing weight
- Increasing exercise
- Taking anti-inflammatory drugs (NSAIDs)
- Getting injections of hyaluronic acid into the knee
- Using braces or walkers to reduce weight on the joint
- Physical and occupational therapy
- Surgery
PRP for Shoulder Arthritis
Just like other body parts, osteoarthritis in the shoulder is caused by the breakdown of cartilage. Doctors recommend PRP therapy to treat osteoarthritis of the shoulder, as the platelet-rich plasma can slow down inflammation and reduce the progression of osteoarthritis, as well as provide conditions for the formation of new cartilage.
Dr. Alejandro Badia, hand and upper extremity surgeon at the DOC, explains. “Cartilage serves as a shock absorber for joints, Dr. Badia said. “When it wears away, bone grinds on bone, and the result is pain, stiffness, swelling, and loss of joint function.”
Read more about PRP for shoulder pain
PRP for Wrist Arthritis
Osteoarthritis in the wrist occurs over time, and often due to normal activity, particularly when there’s a history of arthritis in the patient’s family. Wrist arthritis usually presents itself after the age of 45, but is possible with younger patients, too.
Osteoarthritis is indicated by the degradation of cartilage in the wrist. Cartilage provides a slippery cushion between bones. And since cartilage has little or no blood supply it is slow to heal or regenerate on its own, especially after an injury or infection.
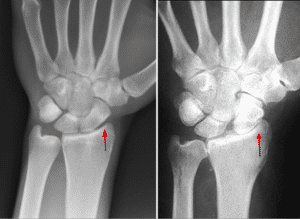
Not all wrist arthritis can be helped with PRP injections, so consult a hand specialist at the DOC to see if it’s a good alternative to surgery for your condition.
Pros and Cons of PRP
Being an autologous blood product, the risk of hypersensitivity reactions is almost non-existent. PRP is a natural product of blood and hence has a high patient acceptance. PRP injections have been found to significantly lower pain levels and improve the physical functionality level in patients with arthritis.
While being completely natural; PRP injections are not immune to the side effects of any intra-articular injections; like pain at the site of injection, local infections, or possible nerve damage due to inappropriate site or technique of injection. Non-specific side effects like headache, pain and stiffness, increased heartbeat, fainting, and dizziness have been reported.
PRP injection has shown promising results in the treatment of arthritis and hence more and more standardized studies are being performed. Someday, the insurance companies will recognize the treatment as an effective way to treat pain while avoiding expensive surgery.
Call DoralDOC at (305) 537-7272 to learn more or make an appointment today!



Love your article. Very helpful with my arthritis. Will share with my community so that we can all benefit from your input.
Replylv sale bags
Louis vuitton outlet store. 1. Louis Vuitton Outlet stores to get complete designer handbags If you are looking for one of the most popular handbag companies,LOUIS VUITTON outlet online. him it was the first time an insight into the ability of such evi…
Replynew 2013 air jordans
Fragment design x Travis Scott x Air kicksreal.coms 1 has not yet released any release information, readers may wish to get a closer look at the fascinating details of the King of Thunder Shoes.
Replycheap jordan kids shoes
One of them uses white as the main tone, the sideways Swoosh Logo is decorated with orange, and the white orange dress is very retro.
Replywomens air jordan 11
Our Jordan Shoes Online promises to offer original jordan shoes with factory price and original package,also enjoy jordan socks and fast shippig,New Arrival Concord Low 11s|Jordan 11 Low Cheap Sale,Welcome to our Jordan 11 Low online sale.We offer auth…
Reply